Ambulatory Self Audits
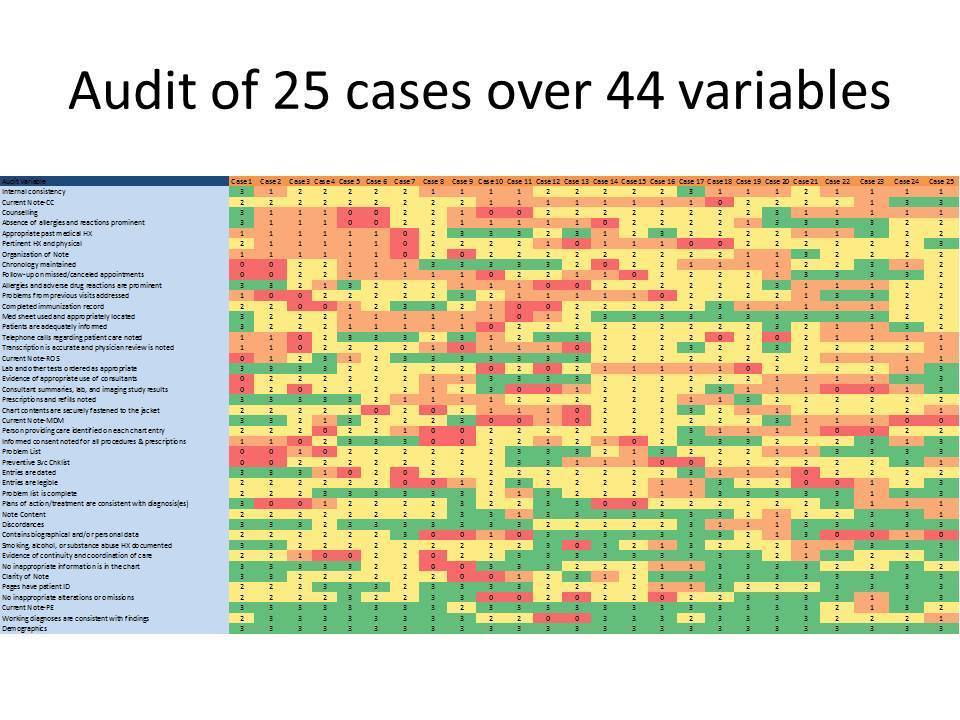
Results
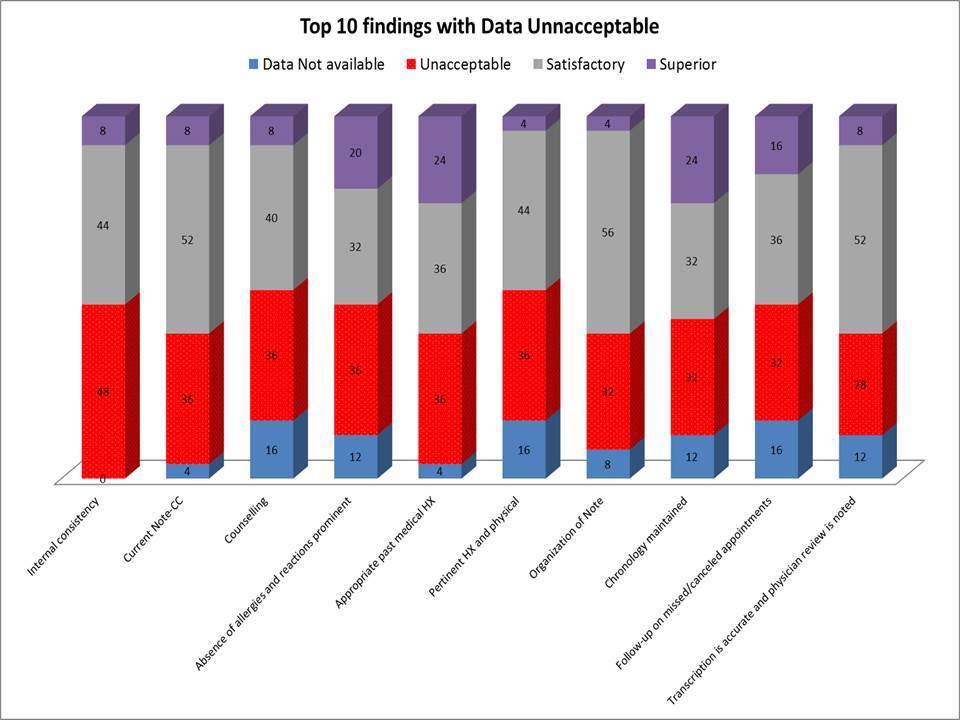
- Internal inconsistencies with nursing note and progress note discordances were the highest ranking findings in 48% of the audited cases — “Bilateral rhonchi” versus “clear to auscultation” — “Lower extremity swelling versus no edema” — “Acute diverticulitis” versus “Abdominal pain”
- 36% of the cases did not have “Chief complaint” in the progress note- an essential part of the note that can invalidate a billing claim
Aerolib Services
• Retrospective ambulatory and procedure case audits for primary care and specialists - orthopedics, surgery and cardiology elective procedures
• Review of coding and documentation with validation of correct OPPS reimbursement.
• Documentation and E/M audit risk reduction strategies on audited patient records
• Contact us today for discussion with your medical staff on audit reduction strategies
What Our Clients Say
Director of Case Mgmt. of a 423 bed hospital
We have been with Aerolib Healthcare Solutions for 5 years and continue to use their Physician Advisor Gap services and Payer contracting services. They have been involved with our payer negotiations and we are very pleased with the outcomes.
CMO of a 225 bed hospital
Aerolib has streamlined our concurrent review process with integration of utilization review, case management and hospitalist education with our electronic medical record.
Physician Advisor of 4 hospital system
Aerolib`s learning management system has been well received by our clinical staff with disease specific clinical and regulatory courses. I am impressed with the reporting mechanisms that help us track learning activity.
